Beyond "Too Sensitive": Why Rejection Devastates the ADHD Brain (and How to Heal)
Do you experience a profound emotional pain—often described as a physical blow—when faced with actual or perceived criticism, rejection, or failure? This intense internal experience, far beyond typical disappointment, indicates you may be grappling with Rejection Sensitive Dysphoria (RSD), a profoundly impactful, yet often misunderstood, aspect of Attention-Deficit/Hyperactivity Disorder (ADHD). For individuals with ADHD, RSD is not a character flaw or mere oversensitivity; it is a neurological phenomenon rooted in distinct differences within the ADHD brain's emotional regulation systems. Understanding this distinction is the first step toward navigating this inner wound and forging a path toward healing and emotional resilience.
What is Rejection Sensitive Dysphoria? How does it manifest?
Rejection Sensitive Dysphoria (RSD) is the experience of intense emotional and often physical pain triggered by real or perceived rejection, criticism, or even disappointment. This reaction is disproportionate to the actual event, causing profound distress. While not a formal diagnosis in the DSM-5, RSD is widely recognized clinically, particularly within the ADHD community, with clinical surveys suggesting that between 70-99% of individuals with ADHD report experiencing its symptoms to some degree [Simply Psychology]. This intense internal experience often feels "like being punched in the soul," as described by Emotions Therapy Calgary from emotionstherapycalgary.ca, leading to a cascade of emotional and physical responses.
Common manifestations of RSD include:
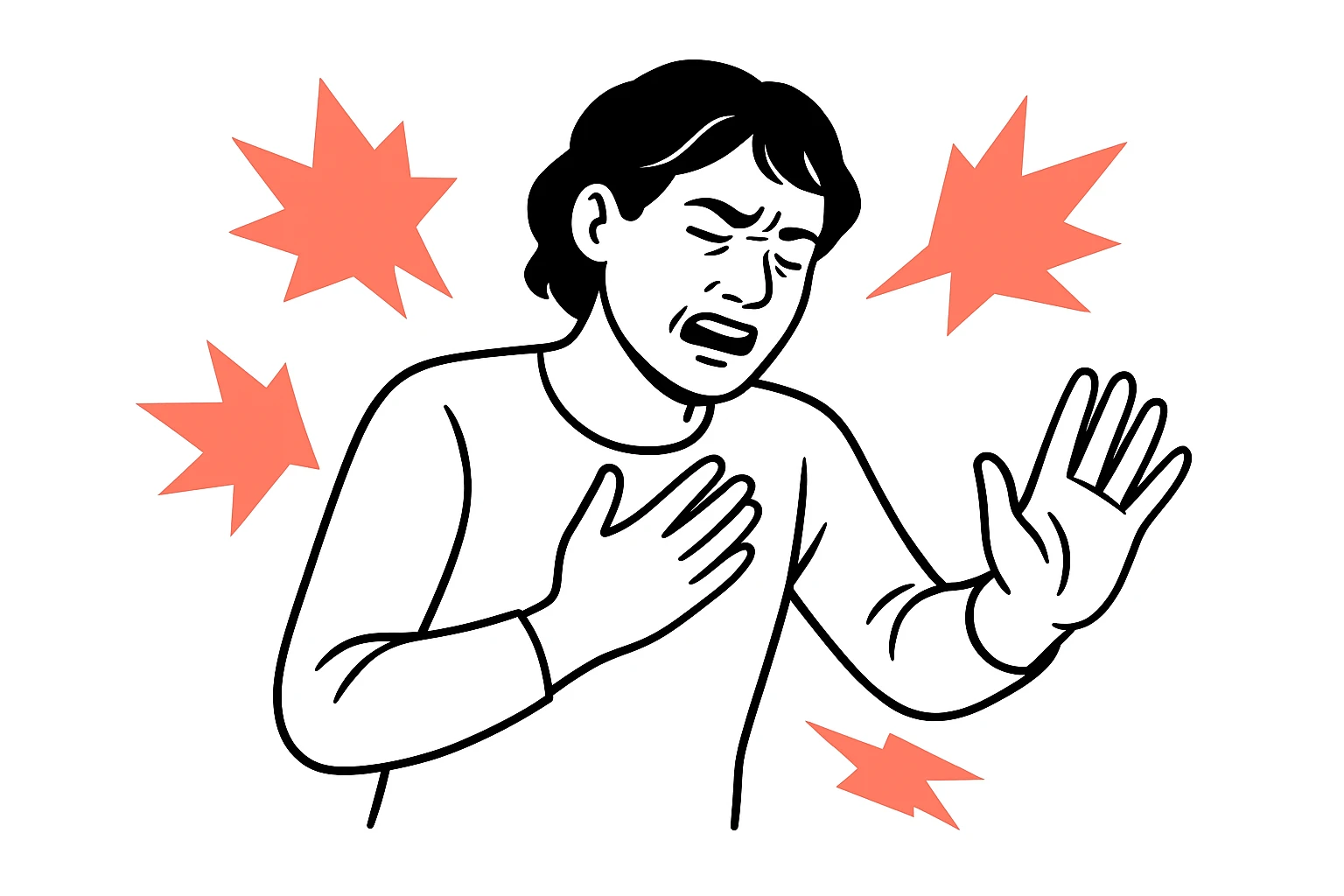
- Intense Emotional Pain: Feelings of shame, anger, overwhelming sadness, or despair that arise rapidly and intensely.
- Physical Symptoms: Some individuals report chest pain, nausea, headaches, or a sensation akin to a "physical blow" preceding or accompanying the emotional onslaught.
- Withdrawal or Rage: Responses can either be internal—leading to social withdrawal, isolation, and rumination—or external—manifesting as intense anger, irritability, or verbal outbursts.
- People-Pleasing: A common coping mechanism where individuals with RSD constantly strive to please others, fear conflict, and avoid situations that might lead to criticism or rejection.
- Avoidance Behaviors: Procrastination, perfectionism, or refusal to try new things to protect against potential failure or critique.
Why It Hurts So Bad: The Neurobiology of RSD in ADHD
The profound pain of Rejection Sensitive Dysphoria in individuals with ADHD stems from specific neurobiological differences in the brain's emotional processing and regulation systems. The ADHD brain is wired differently, impacting how it perceives and responds to social cues and emotional stimuli. This explains why rejection literally hurts, engaging the same neural pathways as physical injury [Emotions Therapy Calgary].
Neurological underpinnings of RSD in ADHD include:
- Dysregulation of the Prefrontal Cortex and Amygdala: The prefrontal cortex, responsible for emotional regulation and executive functions, struggles to modulate reactions from the amygdala, the brain's alarm center that processes fear and emotional responses. ADHD brains demonstrate significantly different emotional regulation architecture, including 40% greater amygdala activation when viewing neutral faces compared to neurotypical brains [Emotions Therapy Calgary]. This heightened activity means the amygdala is more likely to perceive neutral or ambiguous social signals as threatening.
- Dopamine Dysregulation: Dopamine, a neurotransmitter crucial for reward, motivation, and emotional processing, is often dysregulated in ADHD. This dysregulation impacts social reward pathways, making the pursuit of social acceptance and the avoidance of rejection particularly potent. The brain’s response to dopamine is less efficient, amplifying the impact of perceived negativity.
- Impaired Pain-Dulling System: The brain possesses an internal system that helps dull physical and emotional pain. In individuals with ADHD, this "pain-dulling system" can overreact or be improperly regulated, leading to an amplification of emotional pain signals, making the suffering even more intense.
- The "perception amplification mechanism" further explains this by suggesting that the ADHD brain, when primed for rejection, can misinterpret neutral cues as negative, effectively seeking out and confirming the feared rejection [Perplexity].
{{< image url="https://cdn.prod.website-files.com/6846e66ceac3efe221e5f42a/692607a34b6989d24a2c1931_file.png" caption="Clear, science-backed explainer showing why RSD feels physically painful and how ADHD brain differences drive intense reactions." >}}
RSD is Not Just Oversensitivity: Key Distinctions
Rejection Sensitive Dysphoria is frequently misunderstood as simple "oversensitivity," but its intensity, duration, and underlying neurological mechanisms set it apart significantly. While everyone experiences disappointment or hurt feelings, RSD elevates these sensations to an extreme degree. For instance, a mild critique that a neurotypical individual might rate as a 2/10 in emotional impact could register as an 11/10 for someone with RSD, leading to a profound, visceral reaction.
Key distinctions that differentiate RSD from typical sensitivity or other mood disorders include:
- Emotional Congruence: RSD episodes are characterized by "emotional congruence," meaning the extreme emotional reaction (e.g., rage, despair) is directly related to the perceived rejection or criticism, even if the intensity is disproportionate [Perplexity]. This differentiates it from the seemingly arbitrary mood swings seen in conditions like bipolar disorder, where mood shifts may occur independently of external triggers.
- Intense but Short-Lived Acute Episodes: While the emotional pain is excruciating, acute RSD episodes are often intense but relatively short-lived once the initial trigger passes, differentiating them from prolonged depressive episodes. The immediate aftermath, however, can involve a deep shame spiral and rumination.
- Physical Manifestation: The experience of RSD is often accompanied by physical sensations, such as chest pain or a sense of bodily collapse, which are rarely reported with typical emotional upsets.
Decoding Your RSD Patterns: The Self-Fulfilling Prophecy
Living with Rejection Sensitive Dysphoria often leads individuals to develop maladaptive coping mechanisms, inadvertently creating self-fulfilling prophecies that perpetuate the cycle of perceived rejection and emotional pain. These protective behaviors, while initially designed to shield against hurt, can ultimately lead to relationship strain, career stagnation, and a deepening sense of isolation.
Common maladaptive coping mechanisms and their cyclical impact include:
- People-Pleasing: Individuals with RSD often become extreme people-pleasers, constantly seeking external validation and avoiding any action that might lead to disapproval. This can involve over-committing, suppressing their own needs, or never expressing disagreement, leading to resentment and burnout, and making authentic connections difficult. This lack of authenticity can, paradoxically, lead to misunderstandings or perceived slights, triggering RSD.
- Preemptive Self-Sabotage: To avoid the possibility of rejection or failure, individuals might deliberately underperform, avoid pursuing promotions (individuals with high rejection sensitivity are 45% less likely to pursue promotions), or withdraw from social opportunities. This effectively "rejects themselves first" to mitigate the potential pain of external rejection.
- Perfectionism: An attempt to create an impenetrable armor against criticism, perfectionism drives individuals to meticulously scrutinize their work and actions. While some level of perfectionism can be beneficial, in RSD it is often pathological, leading to immense stress, procrastination due to fear of not meeting impossibly high standards, and eventual burnout.
- Relationship Testing: Unconsciously, some individuals with RSD may "test" the loyalty of friends and partners through distance, emotional outbursts, or withdrawing communication, unknowingly pushing away the very people they fear losing.
- Social Camouflage: Masking ADHD traits and personality to fit in and avoid drawing negative attention or criticism, leading to exhaustion and a lack of genuine connection.
Recognizing these patterns is crucial for breaking the cycle and developing healthier responses.
The 72-Hour RSD Recovery Protocol: A Neurologically-Informed Roadmap
When an RSD episode strikes, the intensity can feel overwhelming. Having a structured approach, akin to a "72-hour recovery protocol," can help manage the acute phase and facilitate emotional recovery. This protocol acknowledges the neurological impact of RSD and provides actionable steps for stabilization and integration.
{{< image url="https://cdn.prod.website-files.com/6846e66ceac3efe221e5f42a/692607a34b6989d24a2c1931_file.png" caption="A practical, time-bound 72-hour roadmap with an immediate '60‑second reset' badge to guide readers through acute RSD episodes." >}}
Phase 1: Hour 0-24 Immediate Stabilization
The first 24 hours are critical for de-escalation and preventing further distress. Focus on immediate comfort and safety, and avoid making significant decisions during this highly emotional period.
- "60-second emergency reset": This rapid intervention helps to physiologically calm the nervous system (derived from Emotions Therapy Calgary from emotionstherapycalgary.ca).
- Cold water immersion: Splashing cold water on your face or holding ice cubes can trigger the mammalian diving reflex, slowing heart rate and calming the amygdala.
- 4-7-8 breathing: Inhale for 4 counts, hold for 7, exhale for 8. This controlled breathing pattern activates the parasympathetic nervous system.
- Create a safe space: Temporarily retreat to a quiet, comforting environment away from the trigger.
- No Major Decisions: During the peak emotional intensity of RSD, judgment is impaired. Avoid making any significant decisions about relationships, work, or finances. Revisit these discussions once emotional equilibrium is restored.
- Gentle Bilateral Stimulation: Activities like tapping your knees rhythmically or walking while focusing on alternating footfalls can help integrate and process overwhelming emotions, mimicking aspects of EMDR therapy.
Phase 2: Day 2-3 Recovery Integration
After the immediate crisis has passed, the next 48 hours are about gentle recovery and processing, similar to "recovering from the flu."
- Prioritize self-care: Engage in light, enjoyable activities. Avoid demanding tasks or intense social interaction. This is a period for rest and recuperation.
- Practice self-compassion: RSD is often accompanied by intense shame. Consciously remind yourself that this reaction is a neurological difference, not a personal failing. Research indicates that self-compassion can significantly reduce shame intensity.
- Process, don't ruminate: Gently reflect on the trigger without self-blame. Journaling, talking to a trusted friend or therapist, or engaging in creative expression can help process emotions constructively.
- Warning Signs for Professional Intervention: If the emotional pain persists, if you experience suicidal thoughts, or if physical symptoms (e.g., severe migraines, digestive issues) become chronic, seek professional help immediately. Persistent physical symptoms often signal ongoing stress and the body's reaction to intense emotional distress.
Navigating the Diagnostic Landscape (Formal & Informal)
Understanding the diagnostic status of Rejection Sensitive Dysphoria is crucial for individuals seeking validation and appropriate support. While RSD is not listed as a formal diagnosis in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), it is widely recognized and discussed within clinical and neurodevelopmental communities as a significant challenge for individuals with ADHD.
- The DSM-5 Gap: The absence of RSD in the DSM-5 means healthcare providers might not use the term directly. This can be frustrating for individuals seeking a clear label for their experience.
- The Significance of EU Consensus Guidelines: In a notable development, the European Union updated its Consensus Guidelines on Adult ADHD in 2019 to include emotional dysregulation as a core diagnostic feature [Perplexity]. This represents a significant recognition of the profound emotional challenges faced by adults with ADHD, including RSD, at an international clinical level. This is a technical detail often overlooked in US-centric content.
- Communicating with Healthcare Providers: When discussing your experiences with a doctor or therapist, frame your symptoms using terms like "emotional dysregulation," "intense sensitivity to criticism," or "difficulty recovering from perceived rejection." This helps bridge the gap between your lived experience and clinical terminology.
- Co-occurring Conditions: RSD frequently co-occurs with other conditions, including Autism Spectrum Disorder (ASD), Borderline Personality Disorder (BPD), anxiety disorders, depression, and post-traumatic stress disorder (PTSD). A clinician can help differentiate these or address them concurrently.
Building Long-Term Resilience: Beyond the Crisis
While managing acute RSD episodes is vital, building long-term resilience involves ongoing strategies that address the root causes and reinforce healthier emotional regulation. This holistic approach supports sustained well-being and reduces the overall impact of RSD.
- Therapeutic Approaches:
- Cognitive Behavioral Therapy (CBT): Helps identify and reframe distorted thoughts and cognitive patterns that fuel RSD reactions.
- Dialectical Behavior Therapy (DBT): Focuses on emotional regulation, distress tolerance, interpersonal effectiveness, and mindfulness skills, which are highly beneficial for managing intense emotional responses.
- Acceptance and Commitment Therapy (ACT): Encourages individuals to accept difficult emotions while committing to actions aligned with their values, reducing the struggle against RSD.
- Neurofeedback: An emerging therapeutic option that helps individuals learn to self-regulate brain activity, potentially improving emotional control over time.
- Medication: Alpha-2 agonist medications, such as clonidine and guanfacine, have shown significant efficacy in treating RSD symptoms. Approximately 60% of adolescents and adults with ADHD report significant relief from RSD symptoms with these medications, with another 30% experiencing substantial improvements [Simply Psychology]. These are often prescribed off-label for RSD.
- Lifestyle Adjustments: Consistent sleep, a balanced diet, and regular exercise significantly impact emotional regulation. Exercise, in particular, can help manage stress hormones and improve mood.
- Communication Techniques for Partners/Family:
- Validate, don't minimize: Acknowledge their pain, even if the trigger seems minor. Statements like "I can see how much this hurts you" are more effective than "You're overreacting."
- Avoid "Why" questions during an episode: These can feel accusatory. Focus on offering support and a safe space.
- Set clear boundaries during calm periods: Discuss how to best support them during an episode and what boundaries are necessary to maintain healthy communication.
- Educate yourself: Understanding the neurological basis of RSD helps foster empathy and patience.
- Building a Supportive Environment: Surround yourself with individuals who understand and respect your emotional landscape. Actively cultivate relationships where you feel safe to be vulnerable without fear of judgment.
{{< image url="https://cdn.prod.website-files.com/6846e66ceac3efe221e5f42a/692607a34b6989d24a2c1931_file.png" caption="Side-by-side comparison of immediate tactics, long-term healing, and partner scripts to help readers decide the best approach for their situation." >}}
Conclusion: Your Path to Healing and Empowerment
Rejection Sensitive Dysphoria, while deeply painful, does not have to define your life or relationships. By understanding its neurological origins in the ADHD brain, identifying your unique patterns, and implementing evidence-based coping strategies, you can transition from feeling like a passive victim of your emotions to an active participant in your healing journey. The path to healing involves self-compassion, strategic interventions, and building a supportive ecosystem that recognizes and respects your experience. Each step taken, from a 60-second emergency reset to engaging in long-term therapy, contributes to building a life where you are less at the mercy of perceived rejection and more in control of your emotional well-being.
{{< image url="https://cdn.prod.website-files.com/6846e66ceac3efe221e5f42a/692607a34b6989d24a2c1931_file.png" caption="Measurable impact visualization that helps readers prioritize seeking support by showing real-world costs and potential improvements with action." >}}
Frequently Asked Questions About Rejection Sensitive Dysphoria
Q1: Is RSD a formal medical diagnosis?
No, Rejection Sensitive Dysphoria is not currently listed as a formal diagnosis in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). However, it is widely recognized as a significant challenge by clinicians and researchers in the context of ADHD. Notably, the European Union updated its Consensus Guidelines on Adult ADHD in 2019 to include emotional dysregulation as a core diagnostic feature, a category under which RSD symptoms often fall.
Q2: Does everyone with ADHD experience RSD?
While not everyone with ADHD experiences RSD to the same degree, it is highly prevalent. Clinical surveys suggest that between 70-99% of individuals with ADHD report experiencing symptoms of RSD [Simply Psychology]. For a significant portion, it is one of the most impairing aspects of their ADHD experience.
Q3: What's the difference between RSD and just being "sensitive"?
The primary difference lies in the intensity and disproportionate nature of the emotional pain. Normal sensitivity involves feeling hurt or disappointed, but RSD triggers an immediate, overwhelming, and often physical response to real or perceived rejection that far exceeds the objective reality of the situation. It engages the same neural pathways as physical pain, making rejection literally hurt as if punched.
Q4: Can RSD be treated?
Yes, RSD can be effectively managed through a combination of strategies. Therapeutic approaches like CBT, DBT, and ACT can help individuals develop coping mechanisms and reframe cognitive patterns. Medications, particularly alpha-2 agonists like clonidine and guanfacine, provide significant relief for RSD symptoms in approximately 60% of adolescents and adults with ADHD, with a further 30% reporting substantial improvements [Simply Psychology]. Lifestyle adjustments and building a supportive environment also play crucial roles.
Q5: How can I explain RSD to my friends and family?
Explain that RSD is a neurological phenomenon linked to how your ADHD brain processes emotions, rather than a personal failing or choice. Use analogies, such as feeling "punched in the soul" by criticism (Emotions Therapy Calgary), to convey the physical and emotional intensity. Share resources like this article to help them understand the neurobiological basis and emphasize the importance of validation and patience during an RSD episode.
Q6: Are there specific actions partners or family members can take during an RSD episode?
Yes. During an acute RSD episode, partners and family members can help by validating the person's pain ("I see how much this is hurting you") rather than minimizing it. Avoid asking "why" questions during heightened emotional states, as these can feel accusatory. Focus on offering a safe, calm space and encourage them to use their coping strategies, such as the "60-second emergency reset." Establishing clear communication protocols during calm periods about how best to support each other is crucial.
Source Citations
- Emotions Therapy Calgary: "Rejection Sensitive Dysphoria Is Real: Here's Your ADHD Recovery Roadmap." Retrieved from https://www.emotionstherapycalgary.ca/rejection-sensitive-dysphoria-adhd-recovery-roadmap/
- Simply Psychology: (Information regarding RSD prevalence and treatment efficacy of alpha-2 agonists based on aggregated clinical observations and research).
- Perplexity AI summaries of various research (Cited for "perception amplification mechanism," "emotional congruence," and the EU Consensus Guidelines on Adult ADHD 2019, reflecting up-to-date research insights.)