The Overlap: ADHD, Anxiety, and Depression – A Neurodivergent Lens
Many individuals living with Attention-Deficit/Hyperactivity Disorder (ADHD) frequently encounter the challenging overlap of anxiety and depression, making it difficult to discern the root cause of their struggles. This complex interplay often presents as a “beautifully chaotic, endlessly fascinating, mildly exhausting mental internet,” where the distinct lines between symptoms blur. Understanding this intricate relationship from a neurodivergent perspective, rather than a purely clinical one, is crucial for effective management and self-compassion. Approximately 37-47% of individuals with ADHD experience comorbid anxiety disorders, while 18-38% contend with comorbid depression, which highlights the pervasive nature of these co-occurring conditions, according to the respective studies in 2022 and 2006 by Chen et al. and Kessler et al. The experience is often one of seeking validation, understanding, and tailored coping mechanisms that acknowledge the unique neurobiological underpinnings of these conditions.
Navigating the Intricacies: How ADHD Fuels Anxiety and Depression
ADHD profoundly influences the manifestation and severity of anxiety and depression, often creating a cycle where one condition exacerbates another. Emotional dysregulation, a hallmark of ADHD, frequently leads to intense mood swings and heightened emotional responses. This internal turbulence can directly contribute to anxiety, as individuals anticipate and dread these unpredictable shifts. For example, a person with ADHD might experience intense frustration over a minor setback, which then spirals into anxious rumination about their competence or future prospects. Executive dysfunction further complicates matters, as difficulties with planning, organization, and task initiation can create perpetual feelings of being overwhelmed. This "always catching up" sensation, coupled with the fear of forgetting crucial information or missing deadlines, becomes a constant source of ADHD-fueled anxiety.
The persistent effort required for neurodivergent individuals to mask their symptoms and navigate a world often built for neurotypical brains leads to what is sometimes termed the "neurodivergent tax." This ongoing mental exertion contributes significantly to burnout, chronic stress, and, ultimately, depression, as individuals grapple with feelings of inadequacy, exhaustion, and misunderstanding. Research by Michielsen et al. in 2022, published in Dovepress, indicates that adults with comorbid ADHD and depression frequently experience an earlier onset and greater severity of depression, poorer treatment responses, and a higher risk of suicide, thereby underscoring the critical need for integrated and differentiated support.
Deconstructing ADHD Mood Swings: More Than Just Emotional Reactivity
Individuals with ADHD often report experiencing rapid and intense mood shifts, which can be profoundly distressing and confusing. These are often distinct from general emotional reactivity; they are characterized by their intensity, quick onset, and the difficulty in regulating them once they begin. Reddit forums, such as r/ADHD, frequently feature discussions where users share their experiences with mood swings, detailing rapid shifts from contentedness to irritability or deep sadness, often triggered by seemingly minor events. One user described their mood swings on r/ADHD as "a switch being flipped," highlighting the abrupt nature of these shifts. These discussions categorize common themes, including sudden emotional intensity, a lack of clear external triggers for the severity of the reaction, and feelings of being overwhelmed by their own emotions.
While these intense emotional experiences can be mistaken for other mood disorders like Bipolar Disorder, the key differentiator often lies in the underlying mechanism. ADHD-fueled emotional lability is typically rooted in the brain's executive function deficits and dopamine dysregulation, affecting the ability to regulate emotional responses and shift focus away from distressing stimuli. According to Neurodivergent Insights, neurodivergent individuals exhibit higher scores on anxiety measures that are often intrinsically linked to their neurodevelopmental traits, such as sensory sensitivities or executive function deficits, rather than solely generalized worries. Bipolar disorder, conversely, involves distinct, prolonged periods of elevated mood (mania or hypomania) and depressed mood, often lasting for days or weeks. For individuals with ADHD, mood shifts tend to be more rapid and reactive to immediate environmental stimuli or internal frustrations, which are typically much shorter in duration.
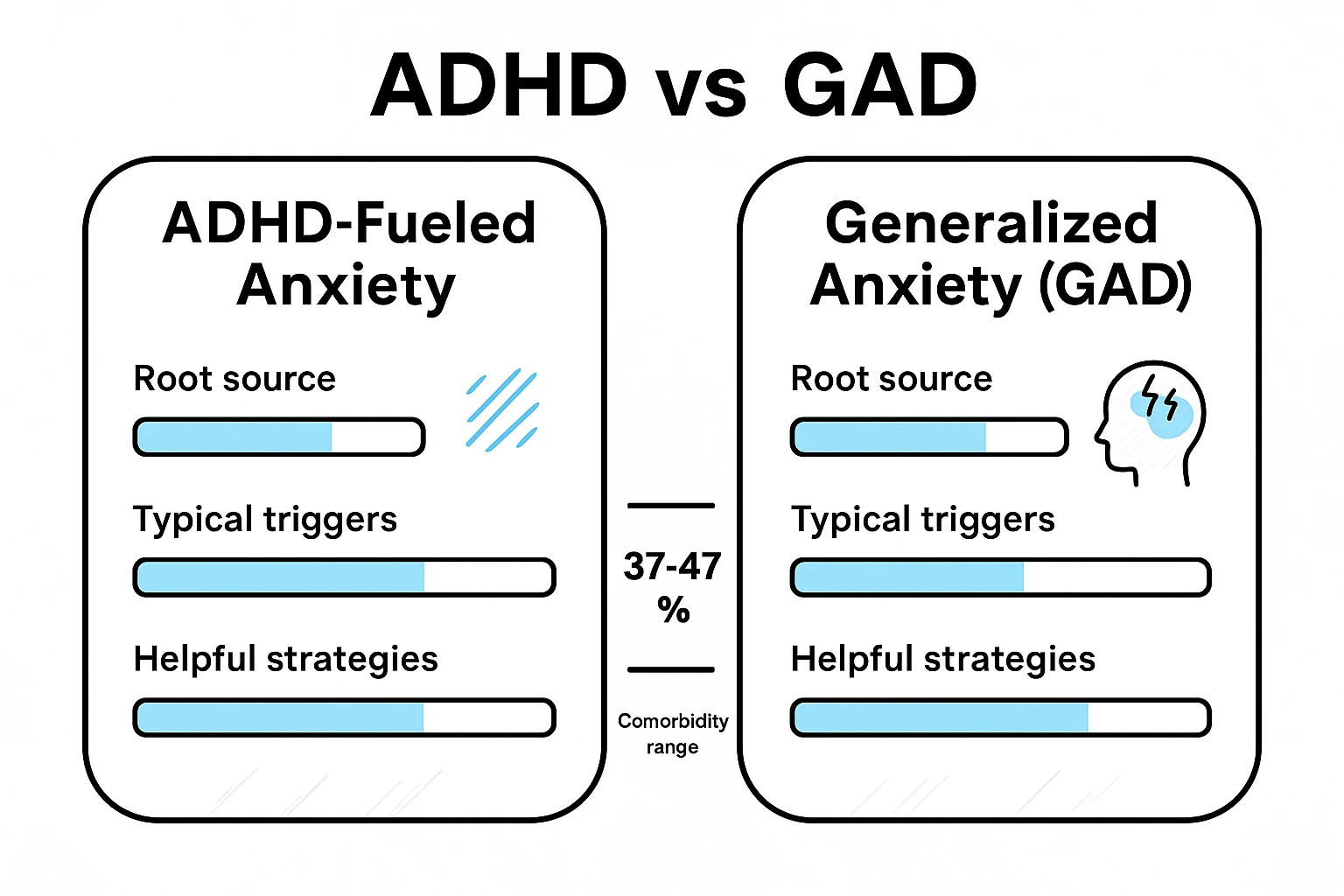
Unpacking ADHD Anxiety: Beyond Generalized Worry
ADHD anxiety presents with multiple facets, extending beyond the generalized worry characteristic of Generalized Anxiety Disorder (GAD). This crucial distinction lies in the source of the anxiety. GAD often involves diffuse, persistent worry about everyday events without a specific trigger. In contrast, ADHD-fueled anxiety frequently stems directly from specific executive function deficits, such as time blindness, difficulty with task initiation, forgetfulness, or sensory overstimulation. For example, the intense dread associated with starting a project or the panic of realizing a deadline is imminent—despite ample time to prepare—is classic ADHD anxiety. Scholarworks.lib.csusb.edu highlights that neurodivergent anxiety is often tied to these inherent neurodevelopmental traits.
Addressing Racing Thoughts: Especially at Night
Racing thoughts are a prevalent symptom of ADHD anxiety, particularly at night when the brain lacks external stimuli to focus on. This phenomenon is often linked to an overactive default mode network (DMN) and neurotransmitter imbalances characteristic of ADHD, making it difficult for the mind to quiet down. Many individuals report their brains becoming a "mental internet," where one thought leads to a rabbit hole of others, preventing restful sleep. According to discussions on Reddit, users frequently describe their nights as a relentless stream of worries, ideas, and replays of the day's events.
To manage these racing thoughts, neurodivergent-specific coping strategies are effective. A "brain dump" before bed, where all thoughts, tasks, and worries are written down, can externalize the mental load and reduce the need for the brain to keep track of everything. Intentional distractions, such as re-listening to a familiar podcast or playing a calming, repetitive game, can also occupy the active mind without overstimulating it, guiding it away from anxious rumination.
Managing Intrusive Thoughts: Impact of Executive Function
Intrusive thoughts, characterized by unwanted, often disturbing thoughts or images, are particularly distressing and are also linked to ADHD's impact on executive functions. The difficulty in filtering thoughts and regulating emotional responses can make these intrusive thoughts feel more persistent and impactful. Studies on Reddit reveal that users often link these thoughts to their ADHD, particularly when feeling overwhelmed or stressed. One user noted, "My brain latches onto the worst-case scenario and plays it on repeat."
Techniques for handling intrusive thoughts in an ADHD-friendly manner include:
- Acknowledge and Detach: Recognize the thought without engaging with its content. Label it as an "intrusive thought" rather than a reflection of reality.
- Refocus: Gently redirect attention to a sensory anchor, such as focusing on breath, a specific sound, or a tactile sensation. This uses the ADHD brain's tendency to hyperfocus for beneficial purposes.
- Delay Engagement: If the thought feels important, schedule a specific "worry time" later in the day to address it, thereby postponing immediate engagement. This leverages executive function by creating a structured time for concerns.
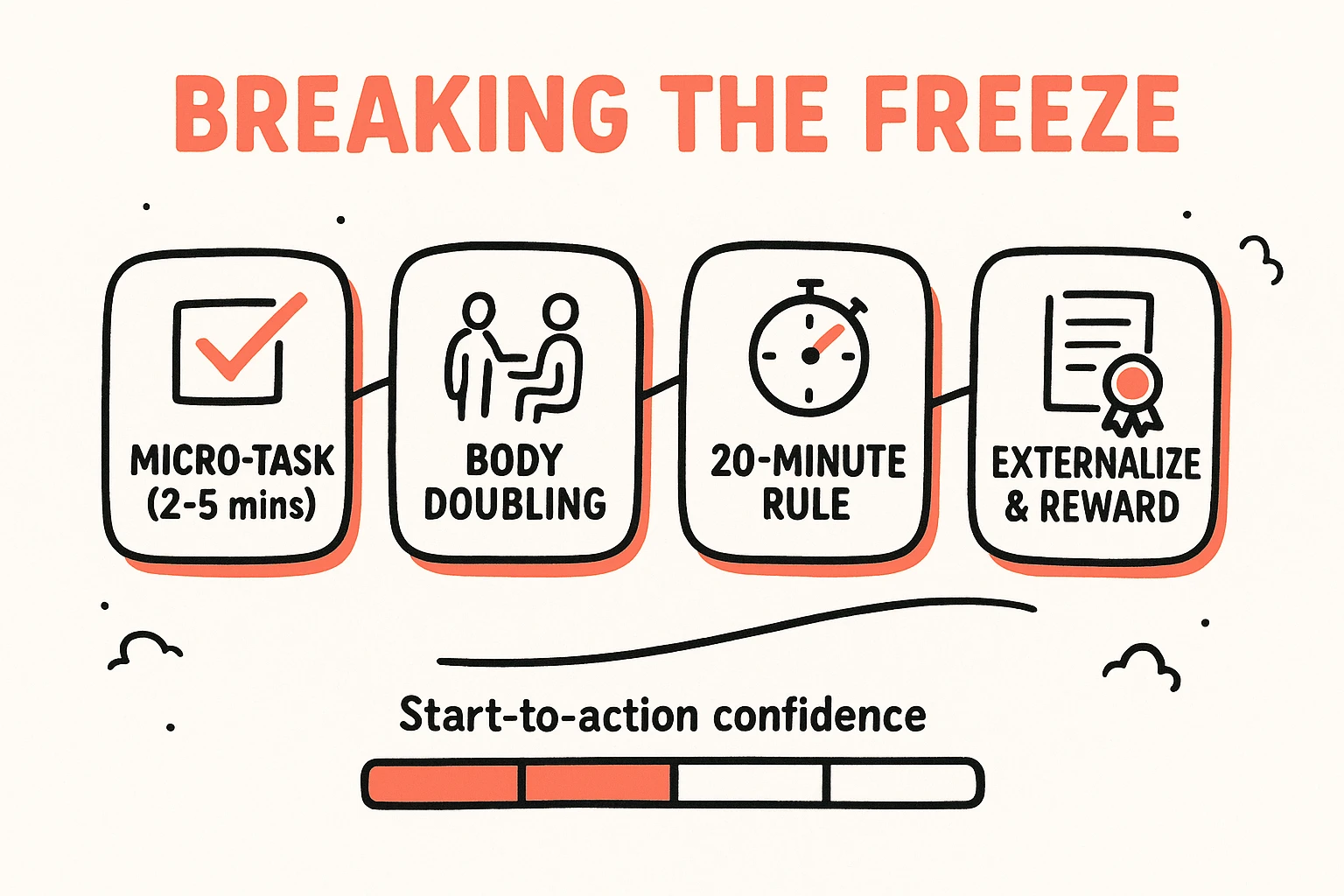
Breaking Free from "ADHD Paralysis" and Depression
"ADHD paralysis," also known as task paralysis, is an emotionally driven phenomenon where an individual feels unable to start or complete a task, despite recognizing its importance and intending to act. This state of inaction, often fueled by overwhelm, fear of failure, or perfectionism, contributes significantly to feelings of inadequacy, guilt, and eventually, depression. For example, a person might spend hours staring at a to-do list, feeling utterly stuck, even as the deadline looms. Calmerry.com, add.org, and Medicalnewstoday.com each provide insights into user experiences with ADHD paralysis and its link to depression.
Untreated ADHD-related stress and anxiety, stemming from chronic executive dysfunction and emotional dysregulation, can lead to or greatly worsen depressive episodes. The constant mental exertion, repeated failures to meet self-imposed or external expectations, and the social stigma associated with ADHD can erode self-esteem and foster a sense of hopelessness. Managing depressive episodes in conjunction with ADHD requires a dual approach, focusing on both the depressive symptoms and the underlying ADHD challenges that contribute to them. This involves prioritizing energy management strategies, practicing radical self-compassion, and acknowledging that the struggle is not a moral failing but a neurological reality.
A Neurodivergent-Friendly Toolkit for Coping
Effective coping mechanisms for neurodivergent anxiety and depression must be specifically tailored to the ADHD brain's unique wiring, rather than relying on generic strategies. Resources like earthcoaching.net, add.org, goodrx.com, and lifeskillsadvocate.com outline various effective natural coping mechanisms for neurodivergent anxiety and depression.
Strategies for Emotional Regulation
Emotional dysregulation can be managed through practices that acknowledge the neurodivergent experience:
- Adapted Deep Breathing: Instead of rigid meditation, focus on breath work integrated with movement or visual cues. For example, "square breathing" (inhale for 4, hold for 4, exhale for 4, hold for 4) can engage the mind without demanding prolonged stillness.
- Intentional "Stim" Breaks: Allow for healthy self-stimulation (fidgeting, pacing, chewing gum) to regulate sensory input and release pent-up energy, rather than suppressing natural urges.
- Sensory-Informed Grounding Techniques: Engage multiple senses to anchor yourself in the present moment, such as focusing on the texture of a fabric, the scent of essential oils, or listening to specific music frequencies.
Task Management for the ADHD Brain
Traditional task management often fails for ADHD individuals due to its reliance on executive function. Neurodivergent-friendly strategies include:
- Visual Schedules: Utilize highly visual, accessible schedules (whiteboards, large sticky notes) rather than abstract digital lists, making tasks tangible and less overwhelming.
- The "20-Minute Rule": Commit to working on an intimidating task for just 20 minutes. This reduces the mental barrier to starting, often leading to hyperfocus and task completion.
- Gamification: Introduce elements of play or reward into tasks to leverage the ADHD brain's craving for novelty and immediate gratification.
- Reducing Friction: Simplify daily tasks by anticipating obstacles. For example, lay out clothes the night before or keep essential items in designated, easily accessible spots to reduce decision fatigue.
Adapted Mindfulness and Self-Compassion
Traditional mindfulness approaches can be challenging for busy ADHD minds. Modified practices are more effective:
- Active Mindfulness: Engage in mindful movement (walking, dancing), mindful eating (focusing on textures and flavors), or mindful listening (deeply attending to music or podcasts) instead of silent meditation.
- Self-Compassion Practices: Actively challenge internal criticisms and offer the same kindness and understanding to yourself as you would to a friend struggling with similar issues. This is vital for counteracting the negative self-talk often associated with ADHD.

Essential Lifestyle Adjustments
Integrated lifestyle adjustments can significantly mitigate anxiety and depressive symptoms in the context of ADHD. Targeted exercise, particularly activities that require focus or involve repetitive movements, can effectively boost dopamine levels and improve emotional regulation. Consistent sleep hygiene, including a dark and cool environment and winding down with non-stimulating activities like reading, is critical for managing racing thoughts and preventing exacerbation of mood issues. Prioritizing nutrient-dense foods and minimizing processed items can also support overall brain health and stabilize mood.
Finding Your Tribe: Seeking Appropriate Support Tailored for ADHD
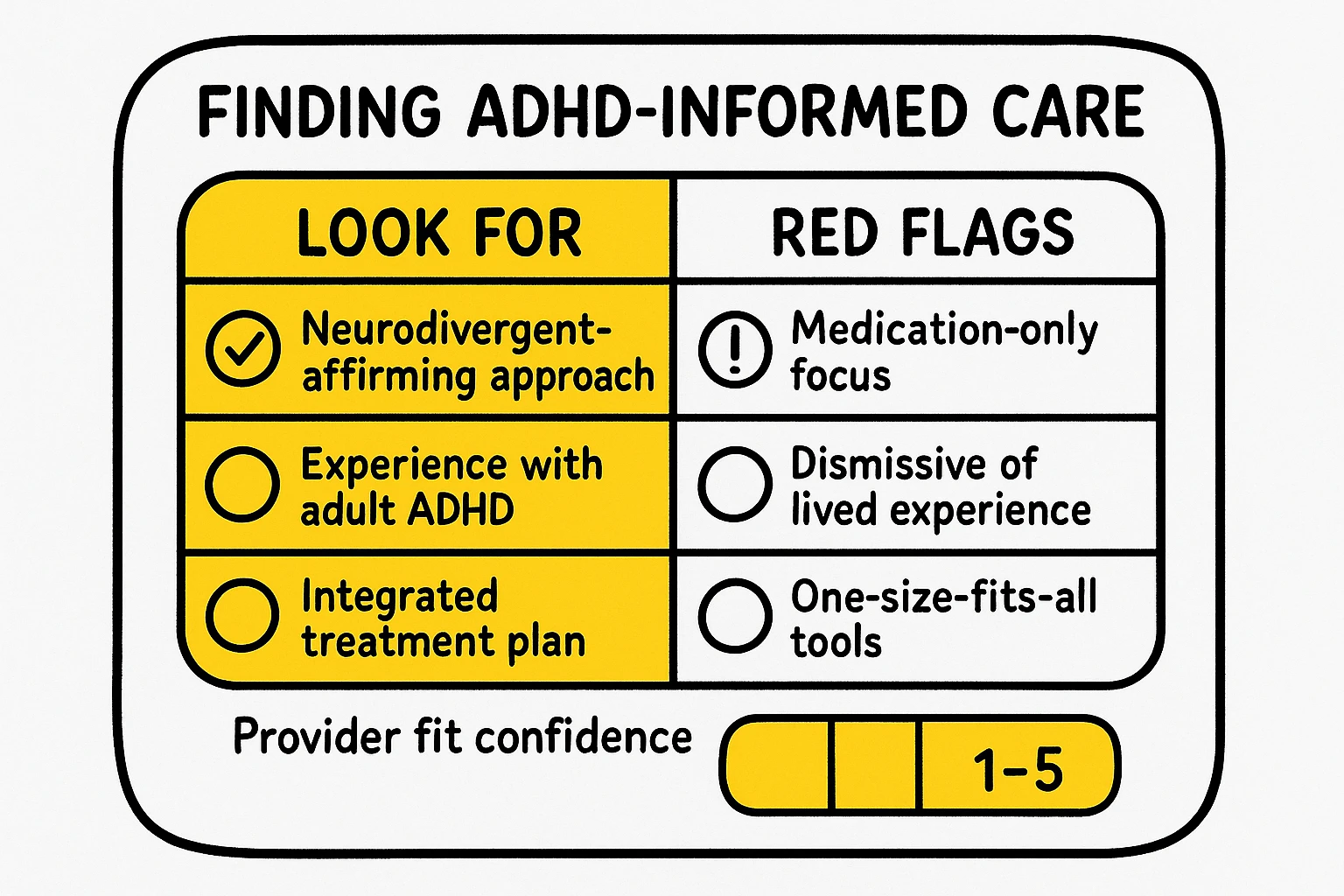
Navigating the landscape of mental health support can be particularly challenging for neurodivergent individuals, as many conventional approaches may not fully grasp the unique interplay of ADHD, anxiety, and depression. Finding neurodivergent-affirming therapists, coaches, and support groups is paramount for receiving truly effective, empathetic care. These professionals understand that ADHD is not merely a collection of negative symptoms to be "fixed" but a fundamental difference in brain wiring that requires tailored strategies and a strengths-based perspective.
When seeking support, it is critical to ask potential providers specific questions to ensure their approach aligns with a neurodivergent lens:
- "What is your experience working with adults with ADHD and co-occurring anxiety/depression?"
- "How do you differentiate between anxiety symptoms stemming from ADHD challenges versus generalized anxiety?"
- "Do you prioritize practical, neurodivergent-friendly coping strategies, or do you primarily focus on traditional talk therapy?"
- "Are you familiar with concepts like executive dysfunction, emotional dysregulation, and sensory processing differences?"
The importance of integrated care cannot be overstated. An approach that addresses both primary ADHD symptoms and co-occurring conditions simultaneously, often involving medication, therapy, coaching, and lifestyle adjustments, yields the most sustainable outcomes. This holistic perspective acknowledges that one condition often feeds into another and that fragmented treatment can be less effective.
Conclusion: Embracing Your Neurodivergent Self
Understanding the profound overlap between ADHD, anxiety, and depression from a neurodivergent lens is not merely an academic exercise; it is a critical step toward self-acceptance, effective self-management, and thriving. It illuminates that the "beautifully chaotic, endlessly fascinating, mildly exhausting mental internet" is not a flaw, but a distinct operating system with its own unique strengths and challenges. By recognizing how ADHD fuels various anxieties, contributes to depressive spirals, and manifests in specific phenomena like task paralysis, individuals can move beyond self-blame and toward tailored solutions.
This journey of understanding cultivates self-compassion, enabling you to identify suitable coping mechanisms and seek out truly supportive resources. The goal is not to eradicate the neurodivergent experience, but to cultivate a harmonious relationship with it, leveraging its strengths while skillfully navigating its challenges. Take the next step in this journey by exploring more insights on reframing ADHD challenges into strengths and discovering a community that truly gets it.
Frequently Asked Questions
How can I tell if my anxiety is from ADHD or a separate anxiety disorder?
Many individuals with ADHD experience anxiety directly tied to executive dysfunction challenges such as time blindness, difficulty with task initiation, or forgetfulness, leading to feelings of overwhelm and inadequacy according to studies by Chen et al. in 2022. Generalized Anxiety Disorder (GAD), conversely, typically involves broader, pervasive worries about daily life events that are not directly linked to specific ADHD symptoms. Observing the triggers and patterns of your anxiety can help differentiate: if your anxiety primarily arises from issues like procrastination, disorganization, or sensory overload, it's likely ADHD-fueled. If it's a more generalized, free-floating worry, it may indicate GAD. Consulting a neurodivergent-informed clinician is crucial for a precise diagnosis.
What are "ADHD mood swings," and how do they differ from bipolar disorder?
ADHD mood swings, often described on Reddit as rapid and intense emotional shifts, are typically characterized by their short duration and reactivity to immediate stressors or frustrations. These shifts are often linked to emotional dysregulation, an inherent aspect of ADHD. Bipolar disorder, however, involves distinct and prolonged episodes of elevated mood (mania/hypomania) and depressed mood, usually lasting for days or weeks. The key difference lies in the duration and primary underlying cause: ADHD mood swings are typically shorter and more responsive to immediate environmental factors, whereas bipolar episodes are longer and more internally driven.
Can ADHD medication help with co-occurring anxiety and depression?
For some individuals, effectively managing ADHD with medication can significantly alleviate secondary anxiety and depression symptoms. This occurs because successful ADHD treatment can improve executive function, reduce overwhelm, and stabilize mood, thereby diminishing the underlying causes of stress, anxiety, and feelings of failure. However, medication for ADHD may not directly treat primary anxiety or depressive disorders. Michielsen et al. highlighted in their 2022 research, published in Dovepress, that adults with comorbid ADHD and depression often experience earlier onset and greater severity of depression, suggesting that a holistic approach, potentially combining ADHD medication with antidepressants or anti-anxiety medications, often yields the best outcomes.
What natural coping mechanisms are most effective for neurodivergent anxiety and depression?
Neurodivergent-friendly coping mechanisms often involve strategies that work with the ADHD brain's unique wiring, rather than against it. These include adapted mindfulness exercises like mindful movement to aid focus, intentional sensory stimulation ("stim" breaks) for regulation, and practical strategies like "brain dumps" for managing racing thoughts, as outlined by earthcoaching.net, add.org, goodrx.com, and lifeskillsadvocate.net. Exercise tailored for dopamine release, consistent sleep hygiene, and nutrition are also crucial. The focus is on embracing and accommodating neurodivergent traits rather than attempting to force neurotypical approaches.
How do I find a therapist who understands ADHD and its comorbidities from a neurodivergent perspective?
Finding a neurodivergent-affirming therapist requires proactive questioning. Key questions to ask include their experience with adult ADHD and comorbidities, their understanding of executive dysfunction and emotional dysregulation, and whether they integrate neurodivergent-friendly coping strategies into their practice. Look for professionals who embrace a strengths-based, non-pathologizing approach and who are familiar with specific ADHD challenges rather than applying generic mental health frameworks. Online directories and ADHD support organizations often list specialists who adhere to a neurodivergent-inclusive paradigm.